The Power of Palliative Care
What one Rare Mom wants you to know about palliative care programs and how they’ve impacted her family.
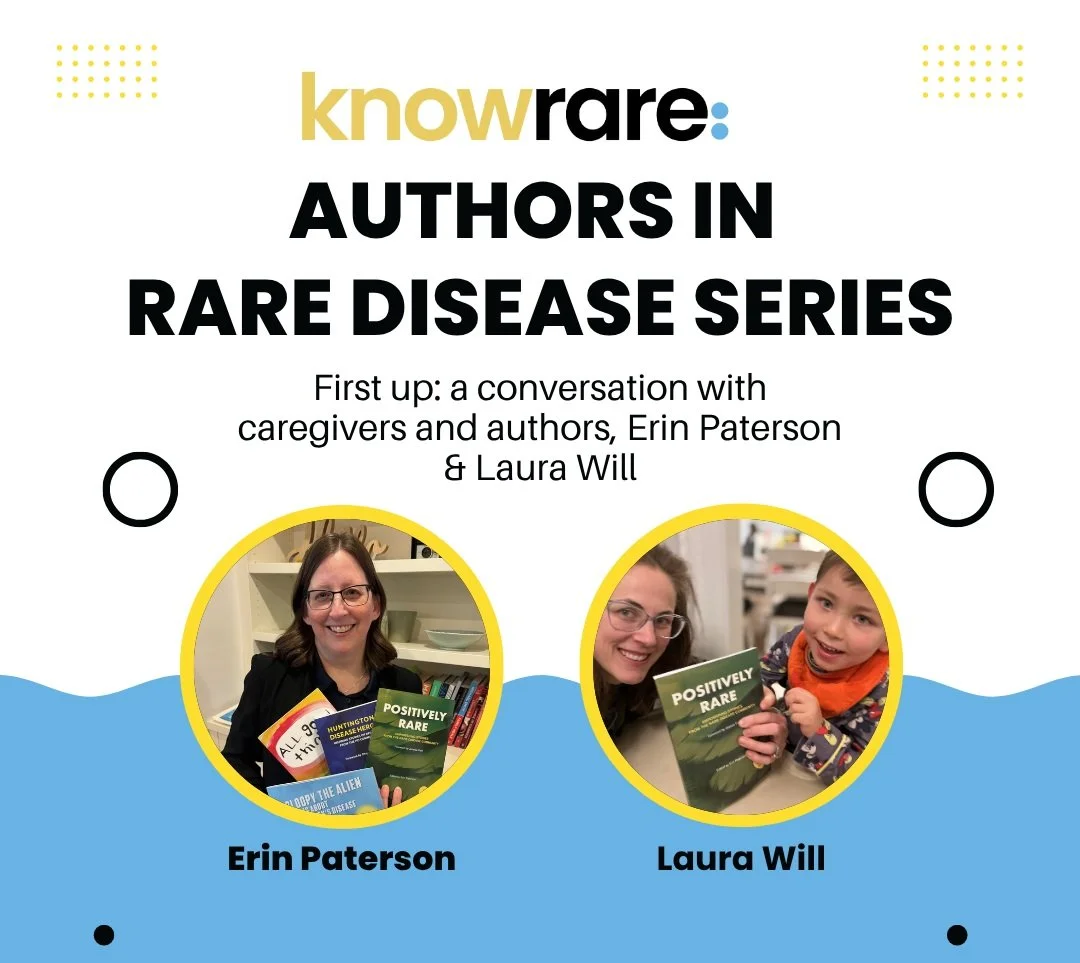
By Laura Will
After a diagnosis, a person with a rare disease—along with their caregivers—can be left scrambling for answers, searching for treatment, and picking up the pieces of their pre-diagnosis life. We reassemble and mend, reprioritize, and move forward with a diagnosis we did not choose. In truth, we have no other choice but to continue with courage and hope. The stresses and symptoms are chronic. We grapple with the social-emotional impacts of the diagnosis on everyone involved. We lay awake, wondering why. It is here, amid the realities of rare disease, symptom burden, and ongoing uncertainty, where palliative care services can provide extraordinary support.
What is palliative care?
Palliative care is distinct from hospice care. It’s important to recognize the difference since they are often lumped together (in part because much of palliative care funding comes through hospice programs, and in part because staff for both services often overlap) However, palliative care is designed to improve the quality of life for people living with serious illnesses and their family members.
Palliative care can be helpful at any stage of illness. While receiving palliative care services, you can also receive other medical treatments intended to cure or treat. Service areas include physical, emotional, social, and spiritual well-being.
“Amid the realities of rare disease, symptom burden, and ongoing uncertainty, palliative care services can provide extraordinary support.”
Palliative care teams may include nurses, social workers, music therapists, art therapists, child life specialists (hear more from a child life specialist here), nutritionists, and spiritual counselors.
Who qualifies for palliative care?
Palliative care is a program encompassing support services for individuals living with medical complexity and/or a life-limiting diagnosis, along with their families. Many programs are covered by state funding, but you should always check with your local palliative care provider for specific details that are relevant to your case.
How can you access palliative care services?
There will be an intake process to determine if you or your loved one qualifies. Your treating physician can also make a referral. You can consult this directory to locate a palliative care program near you.
My perspective on pediatric palliative care
Before my son’s diagnosis, I believed that life was a series of choices. With persistence, attention, education, and a little bit of luck, I thought that I could build the family life I imagined. For better or for worse, my medically complex child taught me that rare parents—and rare patients—do not have such control. That said, palliative care has given me back a sense of control, within the confines of my son’s condition.
I met my palliative care team in May 2020. It was during the one-parent-only COVID rule, inpatient, at Mass General for Children. I was slightly dizzy, holding my four-month-old baby, having just been told that he had been born with a rare brain malformation.
I was shattered. After a lengthy discussion, waves of nausea and utter disbelief, signing papers for genetic testing, and stunned silence, the diagnosing neurologist left the room .As if through an invisible revolving door, the inpatient palliative care team arrived: a doctor, a social worker, and a child-life specialist. Also invisible were the superhero capes. I don’t remember exactly what they said, but I remember one thing I said: “I am worried about me.” For the first four months of my baby’s life, I had been trying to stoically navigate my way through postpartum depression, as well as an acute anxiety that something was just not right with my baby. With this life-altering diagnosis, the darkness was threatening to swallow me whole.
My son was discharged later that day. On shaky legs, I left the hospital, carrying him in his infant car seat that felt like it was made of lead, returning to a family life that seemed absolutely surreal. But within a week, the social worker had connected me with a grief counselor who agreed to see me outside (: we were still at the peak of 2020’s COVID wave). This counselor was a lifeline. During a time when accessing mental health resources was extremely difficult, it was an immense help to have that connection made for me. Together we worked through the acute grief, and the postpartum depression began to recede.
Soon after discharge, my husband and I had a virtual visit with the pediatric palliative care doctor, who was medically informed on our son’s rare presentation. She was able to sit with our uncertainty and guide our emotional understanding of what seizures and other anticipated symptoms might be like. She helped me to open my heart and mind to the beautiful possibilities of a life lived within the confines of this difficult diagnosis. Many months later, when our baby stopped gaining weight due to chronic feeding difficulties, the palliative care physician met with us again to discuss the emotional decision and possible outcomes of surgically placing a G-tube. Her thought process and way of speaking provided a nice contrast to the surgeon’s. Ultimately, we made the decision to move forward with a G-tube placement. Though palliative care would have supported us either way, it has been a wonderful thing.
In addition to the hospital-based palliative care resources, we were referred to the community-based palliative program. A social worker and nurse came to our home for the initial evaluation, where it was determined that we qualified for ongoing services and we discussed what aspects of their programming would benefit our family best. We started with monthly home visits from a child life specialist who would spend time with my daughter: the well-sibling who was young, but perceptive enough to sense the complicated emotions mom and dad were working through as they cared for her baby brother. Additionally, we asked for a music therapist visit once a month— something the kids could enjoy together. As I grieved the sibling relationship I had hoped they would be able to form, these services helped me envision a new one.
“She helped me to open my heart and mind to the beautiful possibilities of a life lived within the confines of this difficult diagnosis.”
Over the years with the palliative care program, we have also enjoyed family outings that allow us to play adaptive sports, and meet other families with their own palliative care needs. We’ve taken family portraits where we get to timestamp our smiles, and I’ve also taken part in an annual Mother’s Day lunch just for mom, where I can be with others who know this unexpected mom life.
We have now had palliative care services in the house for three years, and we see no end to the benefits. My daughter has developed a wonderful, therapeutic relationship with the child life specialist. Music therapy continues to be an hour of silly fun, curated in our home just for us. The quarterly meetings with the social worker and nurse are valuable touch points for me as I manage all the doctors, therapies, decisions, symptoms, advocacy, and normal family growing pains. Each family member is supported and opportunities for joy are created, while challenges (social, emotional, physical, or spiritual) can be understood—and sometimes, overcome.
About Rare Resiliency:
Rare Resiliency is a monthly column written and/or curated by Laura Will. This column explores the concepts and skills that play a protective role against chronic and acute stress. Each article challenges and encourages the reader to continue to develop that inner steadying strength as they face illness and uncertainty, sorrow and joy.